These types of injuries still remain a challenge in their treatment. This is due to a lack of blood vessels in this tissue, making its capacity for self-repair and self-regeneration virtually nil.
The goal of surgical treatment of these injuries is to obtain scar tissue or tissue replacement of histological characteristics as similar as possible with respect to the native tissue.
There are different treatment options for this type of injury. They vary depending on the size and location of the lesion and the age and functional demands of the patient. In all the techniques used, it is essential to define the postoperative rehabilitation protocol, indicating the daily sessions of continuous passive motion and avoiding weight-loading of the operated area so as to favor the formation of scar tissue.
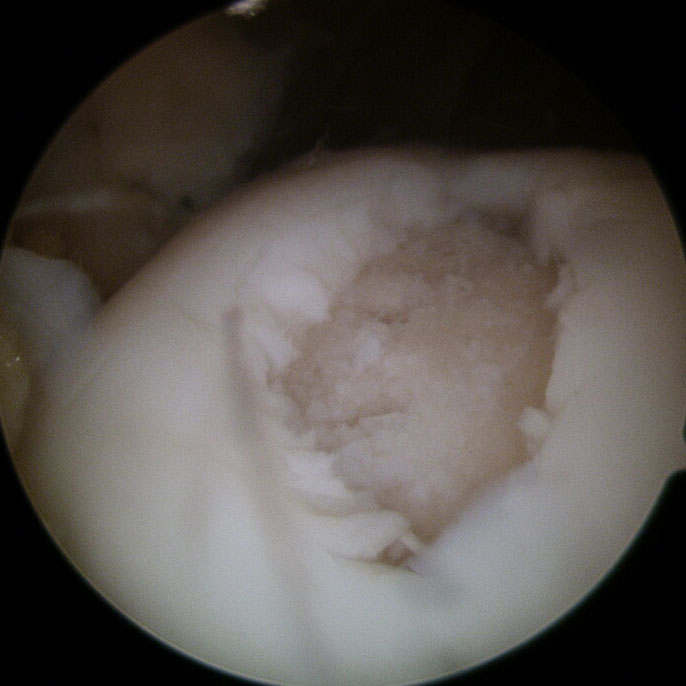
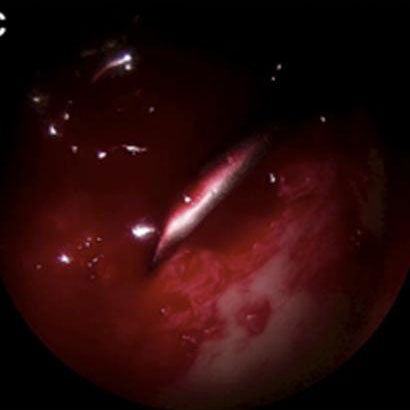
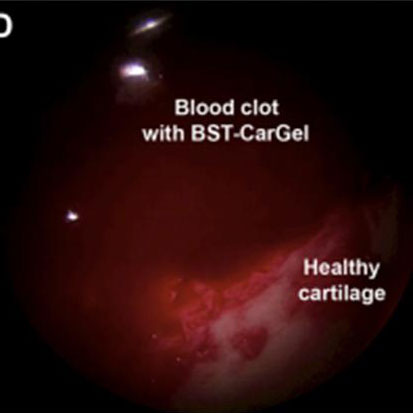
Spinal cord stimulation techniques: microfractures and nanofractures
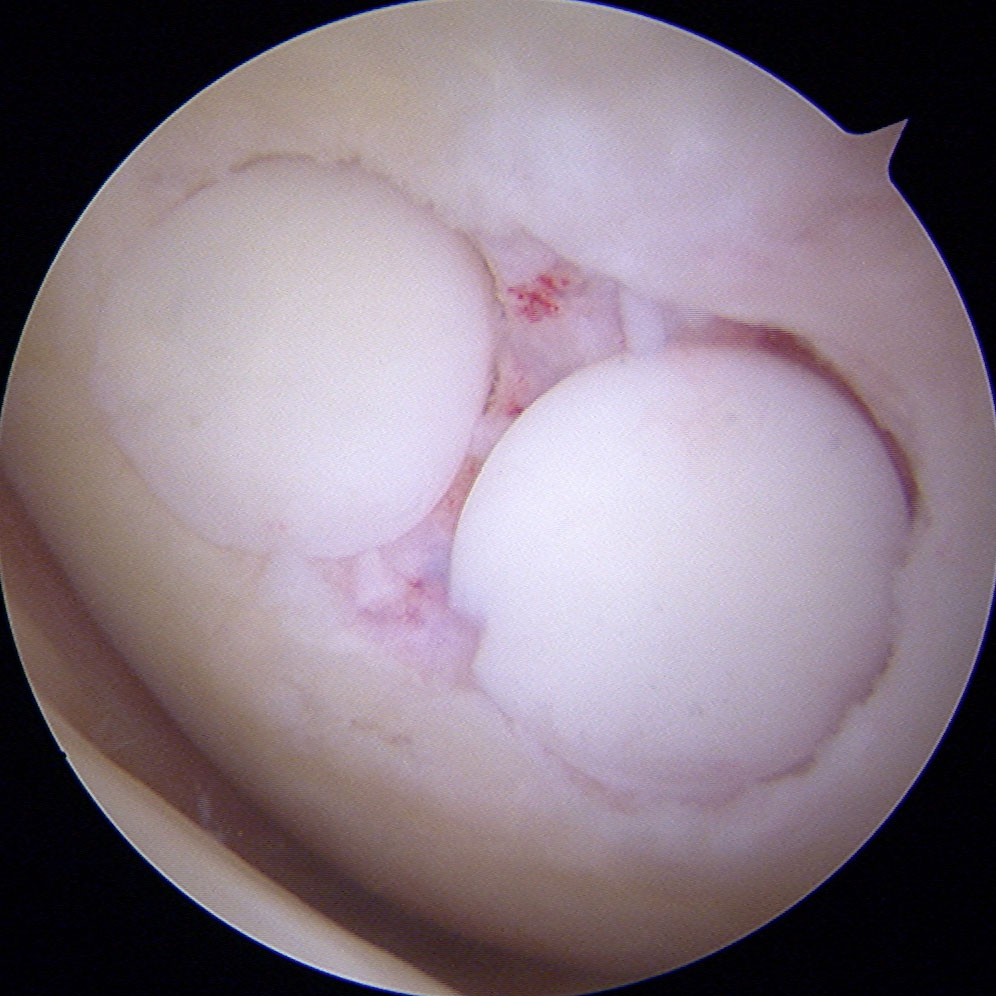
Performing microfractures and nanofractures pave the way for the arrival of stem cells to the area of the chondral injury. These cells have the ability to differentiate and allow for the formation of scar tissue called “fibrocartilage”, which resembles normal hyaline cartilage but has inferior mechanical properties.
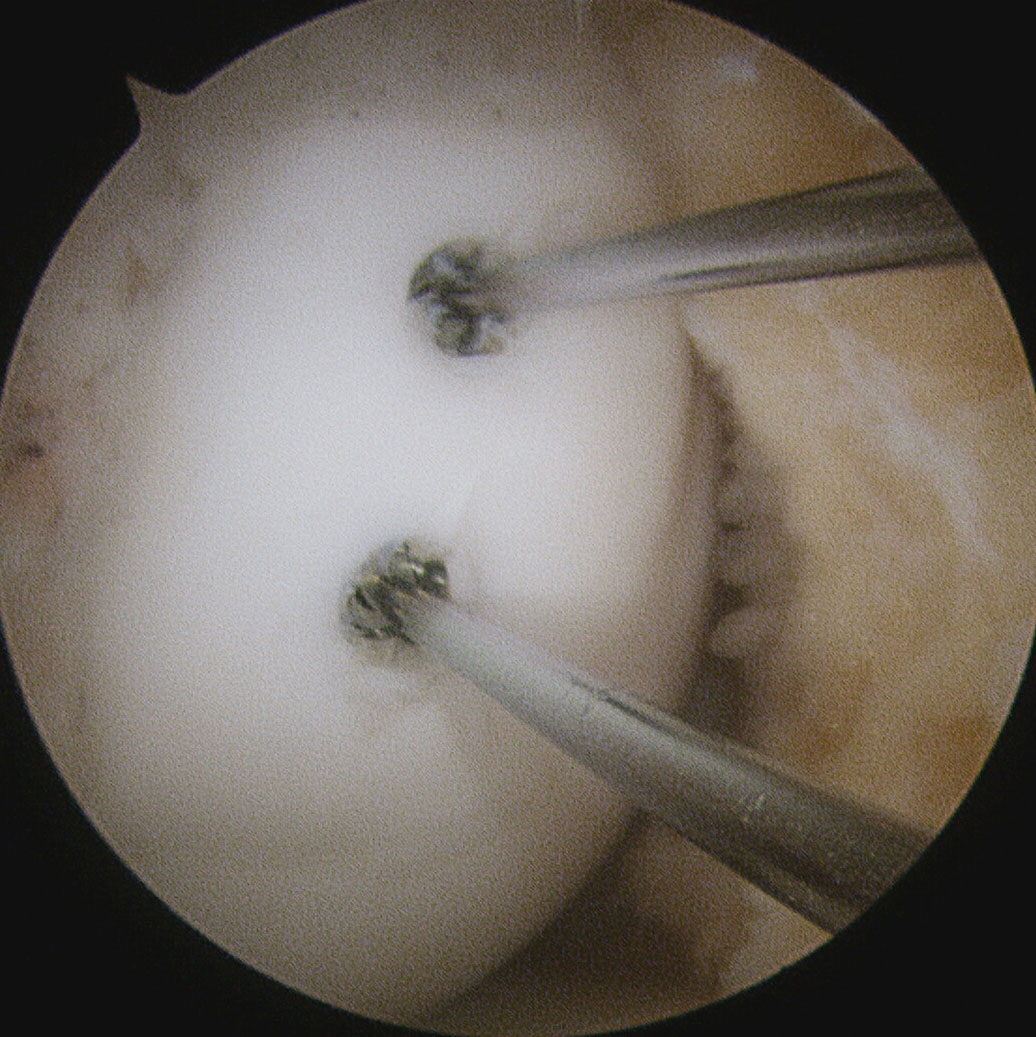
To make for the arrival of stem cells to the injury site, holes are drilled in the subchondral bone (the bone layer exposed in full-thickness chondral injuries).
The difference between microfractures and nanofractures is that the last ones, the most novel, are of smaller diameter and greater depth in order to increase the effectiveness of the technique.
Due to encouraging histological studies, chitosan is used in conjunction with nanofractures. Together, they make for the formation and stabilization of a clot at the level of the area of injury, which will form a tissue with similar characteristics to native hyaline cartilage.
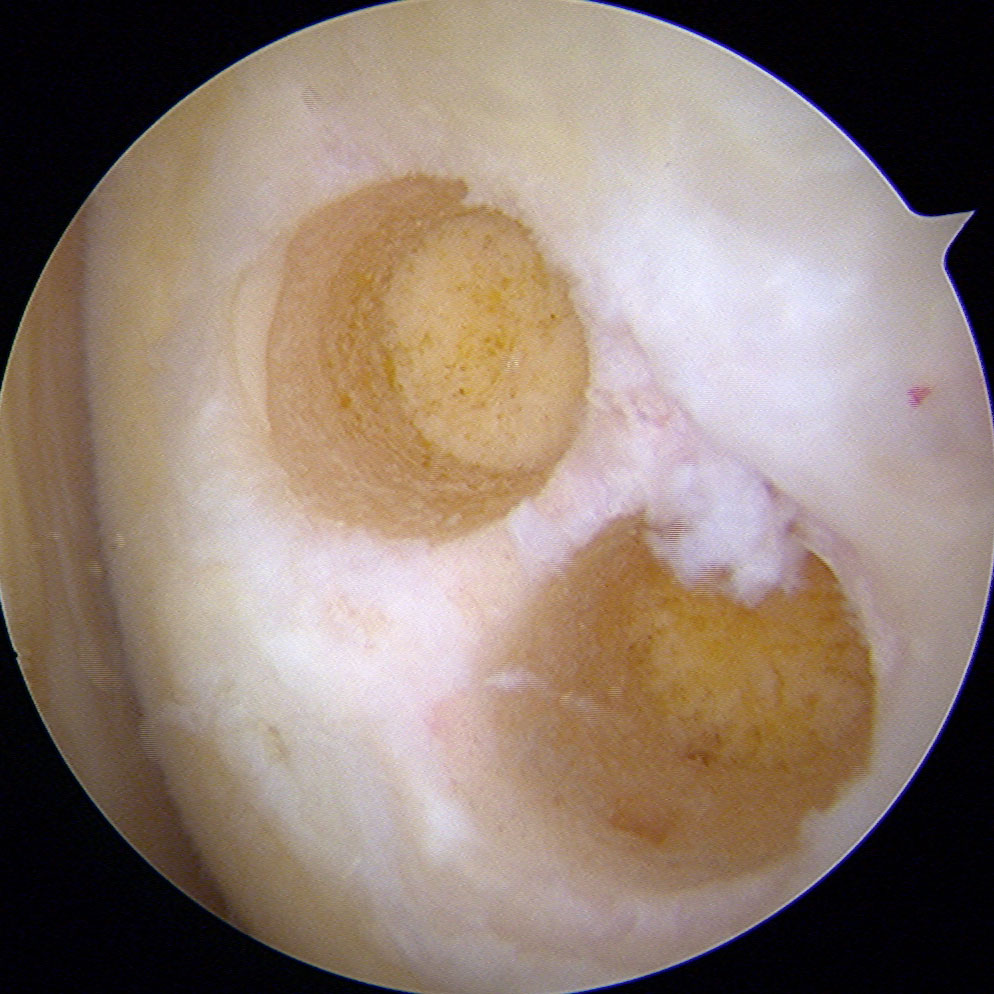
Mosaicplasty
There are cases where injuries, besides affecting the chondral tissue also compromise the subchondral bone. In these situations, the area can be repaired using osteochondral cylinders obtained from areas that do not receive the load on the patient’s own knee.
The realization of this type of intervention will depend on the size and location of the injury and the age of the patient. In larger injuries, the option to use allografts from the tissue bank is reserved.
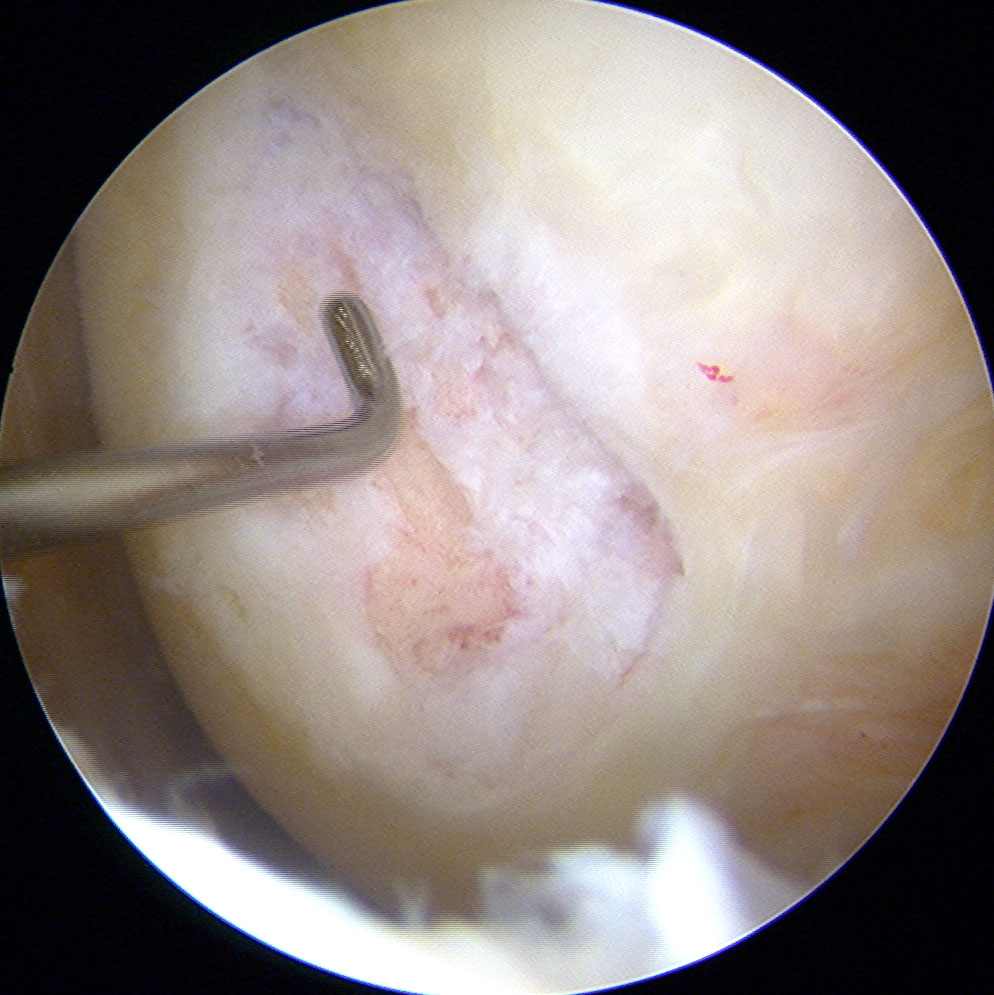
Cultured chondrocytes and mesenchymal cells
This is a technique by which a scar tissue that histologically resembles the original cartilage is obtained. In evaluating clinical results achieved with this technique, it has not shown significant difference to the other techniques mentioned. Therefore, their use is reserved for specific cases.
The chondrocyte culturing calls for two surgical procedures. The first is arthroscopy by which a biopsy of her knee cartilage is taken. This sample is grown in rich mediums to allow for multiplication of the number of cells. After a period of 3-4 weeks, the emplacement of the multiplied chondrocytes in a porous matrix proceeds and they are then implanted in the knee by means of open surgery.
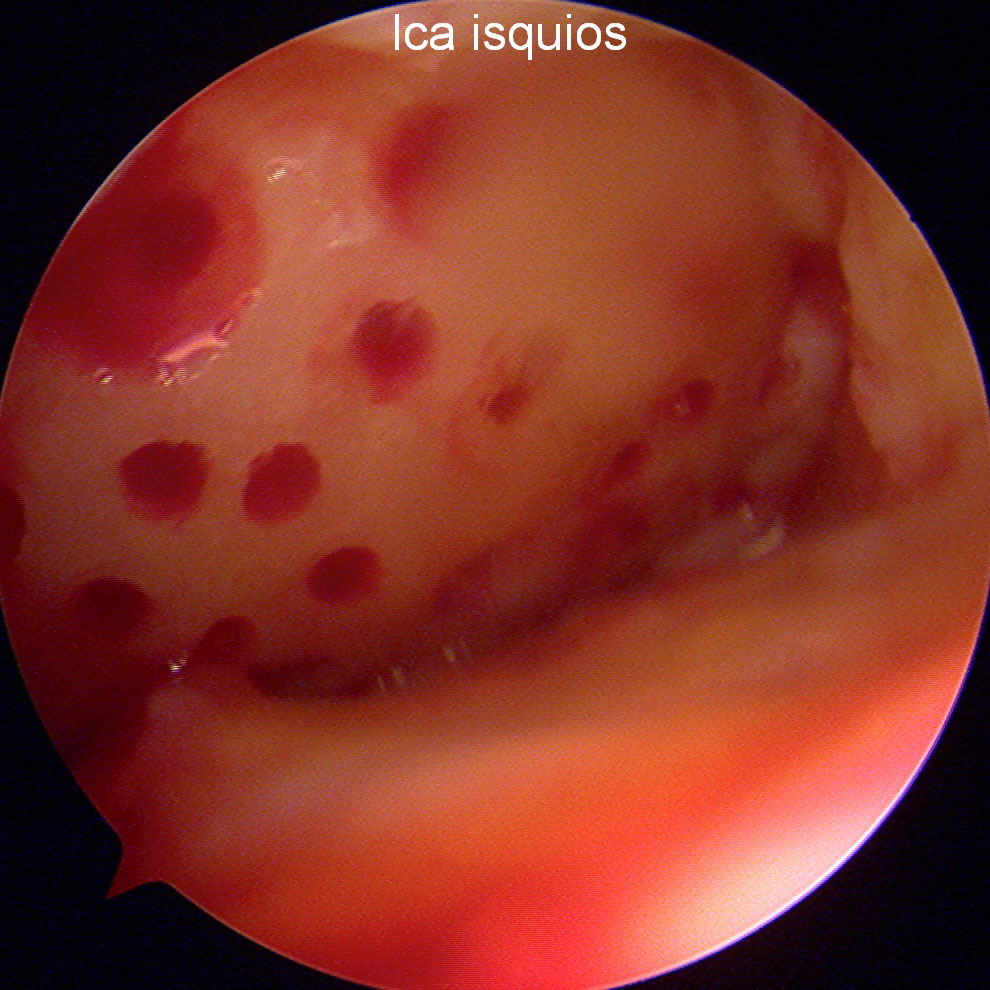
As for the mesenchymal cells, different lines of research and clinical trials to establish and verify their therapeutic ranges are in development in Equilae. They have great potential for differentiation that makes them well-suited to the functionality of chondral cells. They are obtained by needle aspiration of bone marrow, usually performed in the patient’s iliac crest.
Osteosynthesis
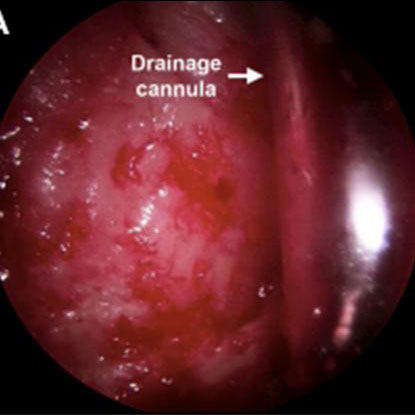
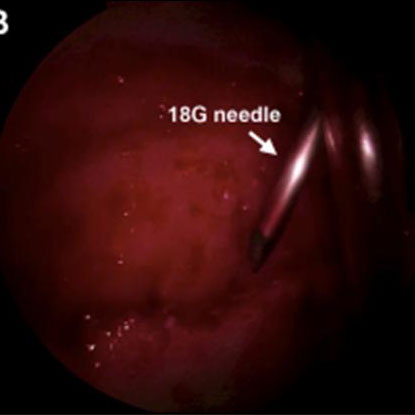
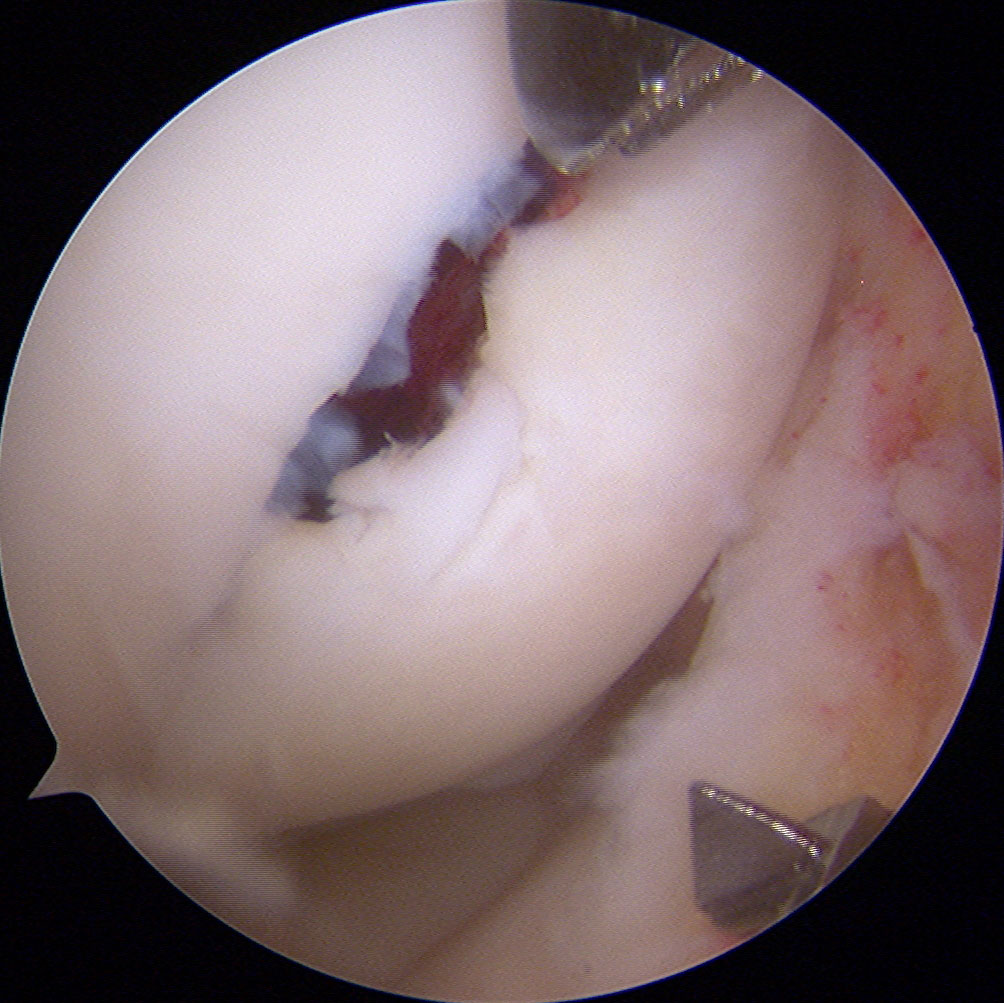
On occasion, detachment of a chondral fragment and its underlying bone may occur. It may be due to trauma or the temporary reduction of the blood supply in the area of the injury, as in osteochondritis dissecans.
Osteochondritis dissecans is a condition that often occurs in adolescents, causing pain and sometimes joint effusion.
In cases where the symptoms do not go away with non-surgical treatments based on the no weight-bearing on the extremity, preparation of the area of the bone defect where the fragment has detached is performed by means of arthroscopy. The aim is to increase the blood supply to the area and later set the osteochondral fragment using different implants, as appropriate.